1 San Diego
20 Escondido
12 Tierrasanta
19 Escondido
2 The Colony, Murrieta
4 Del Mar
5 San Diego
1 La Jolla
2 San Diego
3 Carlsbad
3 Temecula
7 Carlsbad
3 Chula Vista
1 San Diego
1 San Diego
16 Mission Hills
15 Vista
14 Escondido
12 Desert Hot Springs
13 Champagne Village
11 Spring Valley
9 Oaks North, Rancho Bernardo
9 Oceanside
2 Carlsbad
8 San Diego
5 Poway
18 Temecula
6 Riverside
1 Rancho Bernardo
2 Murrieta
Vigorous exercise can slow Parkinson’s by Maggie Fox / Dec.12.2017 / 6:21 AM ET
Vigorous exercise can slow Parkinson’s
by Maggie Fox /

Geoffrey Rogers knew he felt better after hitting the treadmill.
“When I would finish one of the session there would be a calmness. The tremor would be calm,” said Rogers, a 69-year-old Parkinson’s patient.

Rogers was part of a study released Monday that showed intense exercise can slow the progression of Parkinson’s — enough so patients can notice the difference.
It’s the latest study to show that exercise benefits patients with Parkinson’s, and in this case, shows that patients shouldn’t be shy about pushing themselves and getting sweaty.
In fact, the harder they pushed, the better they did, the team reported in the Journal of the American Medical Association’s JAMA Neurology.
“We gave them a proper workout,” said Daniel Corcos, a professor of physical therapy at Northwestern University Feinberg School of Medicine, who helped lead the study.
“If you have Parkinson’s disease and you want to delay the progression of your symptoms, you should exercise three times a week with your heart rate between 80 to 85 percent maximum. It is that simple.”
RELATED: PINEAPPLE PESTICIDE LINKED WITH PARKINSON’S
Rogers pushed himself four to six times a week as part of the study, cranking up the incline on his home treadmill and walking hard. Afterwards, the tremor that is one of the hallmarks of Parkinson’s would subside for a while, he said.
“It might last 20 minutes or more. It’s not a cure; it’s a way to manage the symptoms,” Rogers told NBC News.
It’s clear that exercise is good for Parkinson’s patients, said Dr. Lisa Shulman, who does her own experiments on exercise and Parkinson’s at the University of Maryland School of Medicine
“The evidence is really very strong at this point. There is sufficient evidence now to warrant a general recommendation,” said Shulman, who was not involved in this study.
Parkinson’s symptoms include tremor, rigid muscles and problems with movement. While early treatment can delay the worst symptoms, people almost always get worse. About 60,000 Americans are diagnosed with Parkinson’s disease each year and about a million Americans have Parkinson’s now.
No medical therapy can cure Parkinson’s and while exercise was always shown to help people feel better, it was not generally accepted as a true therapy until recently.
Now teams are trying to find out how much exercise helps and just which symptoms it affects. Doctors say they’d be thrilled just to slow the inevitable worsening of the disease and if they can freeze progression or reverse symptoms, that would be a home run.
Corcos and colleagues say the most intense exercise appears to have at least temporarily frozen symptoms in many of their volunteers.
“The earlier in the disease you intervene, the more likely it is you can prevent the progression of the disease,” Corcos said in a statement.
“We delayed worsening of symptoms for six months,” he added. “Whether we can prevent progression any longer than six months will require further study.”
RELATED: WALKING HELPS PARKINSON’S
They worked with 128 patients with early stage Parkinson’s. They randomly assigned them to either moderate exercise four days a week, intense exercise four days a week, or no additional exercise.
It’s important to randomly assign people, because it’s possible people who voluntarily exercise more or harder also have different symptoms or less severe disease.
The vigorous exercise group were pushed on a treadmill, with the researchers increasing speed and incline until the volunteers were at 80 to 85 percent of their aerobic capacity, meaning they were breathing hard and probably sweating. Rogers was assigned to this group.
“This is not mild stretching. This is high intensity,” Corcos said.
They were trained at the hospital, and then sent home to exercise as part of their daily lives and asked to send their data to the researchers.
“If you have Parkinson’s disease and you want to delay the progression of your symptoms, you should exercise three times a week with your heart rate between 80 to 85 percent maximum.”
“If you have Parkinson’s disease and you want to delay the progression of your symptoms, you should exercise three times a week with your heart rate between 80 to 85 percent maximum.”
The moderate group were pushed to 60 to 65 percent of capacity, which feels like exercise but doesn’t get the heart pumping as hard.
Maximum heart rate is based on age and there’s a formula for calculating exertion. “An estimate of a person’s maximum age-related heart rate can be obtained by subtracting the person’s age from 220,” the Centers for Disease Control and Prevention says.
The maximum heart rate of a 50-year-old person is 170 beats per minute, so 80 percent of that is 136 beats per minute and 60 percent is 102 beats per minute.
RELATED: GUT GERMS AFFECT PARKINSON’S
For some people, a brisk walk will get them to the 80 percent level, while others may need to be running or walking up a steep incline.
The team also assigned people to exercise four days a week with the hope they would actually do it three days a week, for six months. They did indeed get about three days of week of exercise in both groups.
To determine if patients got better or worse, the researchers used the Unified Parkinson’s Disease Rating Scale. The volunteers were on average at about 20 on the scale, which measures 31 different areas of mood, activity levels and motor skills. Patients score from 0-4 on each and thus the most severe possible score is 124.
After six months, those in the high intensity group were still at about 20, on average.
“I was not getting worse. I was not deteriorating during that period of time,” said Rogers, who also did not take any medication during the experiment.
“You could feel it.”
Those taking moderate exercise worsened very slightly — by about 1.5 points on average, which in any single person would not be noticeably worse. Those who did not exercise worsened by three points on average, which is enough for someone to notice, says Shulman.
Shulman did a similar experiment. She found that no matter how intense the exercise, almost all patients who exercised were later able to walk faster.
RELATED: PARKINSON’S PATIENTS DANCE AWAY THEIR SYMPTOMS
“This was counter to our hypothesis. We thought the higher-intensity group would improve the most,” she said.
Shulman and Corcos agree — exercise isn’t just a feel-good thing that Parkinson’s patients can do as a complementary activity. It’s actual medical treatment.
“We are stopping people from getting worse, which is significant, particularly if we catch them early in the disease,” Corcos said.
“I was not getting worse. I was not deteriorating during that period of time.”
“I was not getting worse. I was not deteriorating during that period of time.”
“It’s part of the idea that exercise is medicine.”
Rogers, who owns a construction business, says he failed to keep up with the exercise program when the study ended four years ago, and his Parkinson’s has worsened since.
“The tremor is more intense. It happens more often,” he said. He has no idea if the symptoms would have worsened had he continued to exercise at the same level he did during the six-month-long study.
But it was hard to work and exercise that much, too, he said.
“It was too much. I am going to slow down, which will free up some time for working out more,” Rogers promised.
What Not To Say To Somebody With Dementia
For somebody living with dementia, language and communication can become more difficult over time.
How and when language problems develop will depend on the individual, as well as the type of dementia and the stage it is at. While the person living with the condition may have issues with recall or finding the right word, the words that other people use are important too. A poor choice of language can be both hurtful and frustrating.
Good communication can be key to helping somebody to live well with dementia. Here are a few of the words and questions to avoid in conversation.
7 things not to say to somebody with dementia
- ‘Remember when…?’
While it can be tempting to try and jog the memory of somebody living with dementia, this kind of question is often a reminder of memories lost. This can be a frustrating or painful experience, and there’s also no evidence that training the brain in this way will help somebody hold on to memories. That’s not to say you should avoid talking about the past, but it’s better to lead the conversation and allow the person to join in.
Try this instead:
Instead of posing a question, try leading with ‘I remember when…’ instead. That way the person can search their memory calmly without feeling embarrassed, then join in if they like.
- ‘I’ve just told you that’
Having to answer the same question several times can be frustrating, but repetition will happen. There is little benefit to passing on your frustration to somebody with dementia, and saying ‘I’ve just told you that’ only reminds the person of their condition.
Try this instead:
Try to be polite and as patient as possible. It’s important for somebody with dementia to feel they’re being listened to and understood.
- ‘Your brother died 10 years ago’
A person living with dementia may forget about a past bereavement or ask for somebody who has passed away. But reminding them of a loved one’s death can be painful, even causing them to relive the grief they’ve already experienced. How carers should respond to this may vary for different circumstances, but it’s always good to show sensitivity.
Try this instead:
It may be better to come up with another reason for somebody’s absence, while at other times a gentle reminder is appropriate. In the later stages of dementia, trying to remind them that the person has died is unlikely to work and may be best avoided.
- ‘What did you do this morning?’
Avoid asking too many open-ended questions, as it could be stressful for a person with dementia if they can’t remember the answer. While it might seem polite to ask somebody about their day, it’s better to focus on what’s happening in the present. It’s also important that people with dementia continue to make personal choices, but defining the options might be a helpful technique.
Try this instead:
Rather than ‘what would you like to drink?’, you could ask ‘do you want tea or coffee?’ or more simply, ‘do you want a cup of tea?’.
- ‘Do you recognise me?’
It can be distressing when somebody with dementia doesn’t recognise you, but remember that the feeling is mutual. Asking the person if they know who you are can make them feel guilty if they don’t remember, or offended if they do.
Try this instead:
The way you greet somebody with dementia might change depending on the stage of their condition – judge for yourself, but keep it friendly. A warm hello could suffice, or it may help to say your name.
- ‘Let’s have a cup of tea now, then after that we can go for nice walk and get lunch in that café you like in town.’
Long, complex sentences can be difficult to grasp for somebody with dementia. It’s difficult to process several ideas at once as cognitive abilities slow down, so it’s better to give directions or instructions one step at a time.
Try this instead:
Use short, simple sentences as much as possible. Avoid speaking in loud environments and wait until you have the person’s full attention before you start a conversation.
- ‘Do you need some help with that, love?’
Words like ‘love’, ‘honey’ and ‘dear’ can be patronising for people living with dementia. This is sometimes referred to as ‘elderspeak’ and can cause older people to feel infantilised.
Try this instead:
Always remember the person behind the dementia, using their name as often as appropriate. This helps keep their dignity intact and aids concentration too.
From the Alzheimer’s Society Website
New Stroke Guidelines Extend Time Frame Life Saving Treatment
New stroke guidelines extend time frame for life-saving treatment
by Shamard Charles, MD /
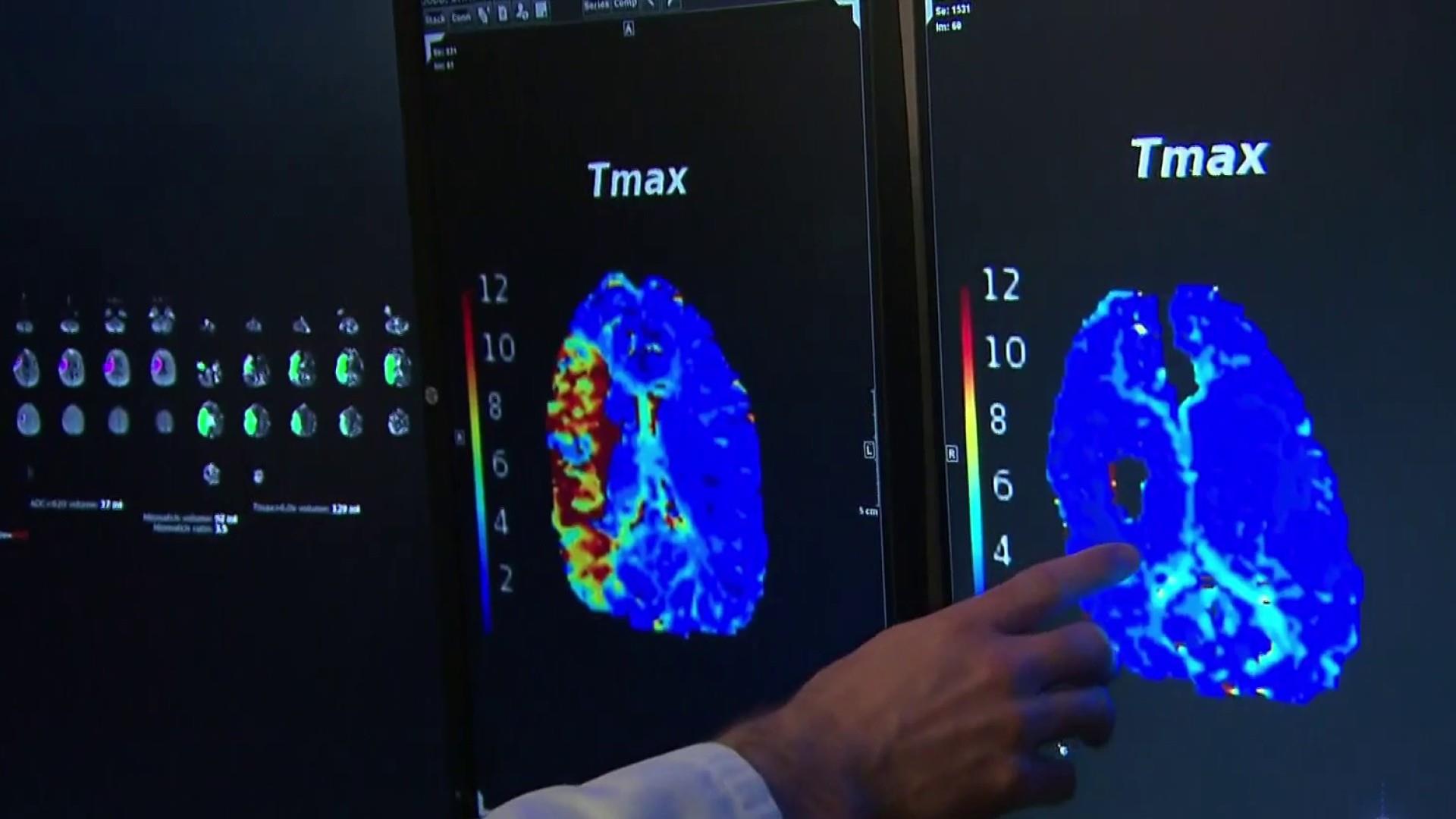
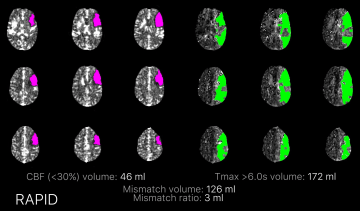
New guidelines on treating stroke suggest that more people could be eligible for life-saving clot removal and treatments, expanding the “golden window” when doctors can minimize or prevent permanent damage from six to 24 hours.
The guidelines, released Wednesday, could completely change the landscape of acute stroke treatment, doctors say — meaning that instead of dying or suffering lifelong disability, one out of three stroke patients could fully recover.
“We now know it’s not so much the amount of time elapsed since a stroke began, as the amount of remaining at-risk but salvageable brain tissue that determines who will benefit from stroke therapy,” said Dr. Gregory Albers, the study’s lead author and director of the Stanford Stroke center.
Eligibility for emergency treatment depends on the time in which the patient first experiences symptoms — so patients who have a stroke in their sleep or are found collapsed in their homes are at greater risk of dying or disability.
A person has a stroke every forty seconds in the U.S. and eighty-five percent of them — roughly 750,000 cases per year — are ischemic, the result of a blockage within a blood vessel supplying blood to the brain. The remaining 15 percent of strokes occur when a blood vessel in the brain tears and blood accumulates in the brain.
Under the new guidelines from the American Heart Association and American Stroke Association, more people who’ve had an ischemic stroke could be eligible for life-saving clot removal and dissolving treatments following ischemic strokes.
The new guidelines recommend an increased treatment window for clot removal from six hours to 24 hours based on brain imaging in select patients and expanded eligibility for clot busting drugs like alteplase (rTPA), the only FDA-approved clot-dissolving treatment for ischemic stroke.
“The expanded time window for mechanical thrombectomy for appropriate patients will allow us to help more patients lower their risk of disability from stroke,” said Dr. William J. Powers, the guideline writing group chair and professor of neurology at the University of North Carolina in Chapel Hill, North Carolina. “That’s a big deal.”
“Implementing these new guidelines is a game changer that will save lives and a tremendous change in the way we will manage this very, very complicated disease.”
“Implementing these new guidelines is a game changer that will save lives and a tremendous change in the way we will manage this very, very complicated disease.”
The new recommendations come as the result of several new studies, including a 38-center clinical trial sponsored by the National Institutes of Health and led by researchers at the Stanford University School of Medicine. Stanford scientists used brain-imaging software to rapidly evaluate — within 2 minutes — blood flow data from incoming patients, the study released Wednesday shows.
Doctors have long viewed the “golden window” — the first few hours after a person starts experiencing stroke symptoms as the time for most effective care.
RELATED: STROKES ON THE RISE AMONG YOUNGER ADULTS, STUDY FINDS
About 300 hospitals around the country already use the new automated brain imaging software, called RAPID, to identify patients who may be candidates for treatment after their 6-hour window has expired.
“I really cannot overstate the size of this effect. The study shows that one out of three patients are saved from the devastation of a stroke, and can walk out of the hospital, completely recovered,” said Dr. Walter Koroshetz, director of the National Institute of Neurological Disorders and Stroke. “The results of the trial were astounding and will have an immediate impact in the clinic and will help us save many lives.”
The new software analyzes perfusion CT or MRI scans to look for significant areas of blood flow in the brain. “This allows doctors to determine what tissue is salvageable. If there is enough salvageable tissue, doctors have more time to treat patients using newer conventional means,” said Albers.
RELATED: NEW STROKE TREATMENT SAVES LIVES, IMPROVES RECOVERY
The new technology saved Cynthia Dodd, a 46-year-old graphic designer from Salinas, California. In April, 2017, Dodd went to bed around 10:30 p.m., anticipating a 5 a.m. wake-up by her husband.

Instead, she woke mumbling and the left side of her body was paralyzed.
“I started to speak to him I knew what I was trying to say in my mind, but it had nothing to do with the sounds that were coming out of my mouth,” Dodd said.
Her husband, Rick Dodd, rushed her to Salinas Valley Memorial Hospital, but she was outside the timeframe for conventional therapy.
An emergency physician told Dodd’s husband about the ongoing Stanford trial — within 45 minutes, she was in a helicopter on her way to Stanford Hospital.
By the time Dodd’s husband and 17 year old son, arrived to Stanford from Salinas, she was already out of surgery. Seven days later she was discharged.
“I am literally standing on this Earth as a wife and a mother because of that procedure,” said Dodd.
Now she is almost fully recovered — talking, walking and driving as before, and plans to return to work in March.
Doctors hope this becomes the norm.
“Implementing these new guidelines is a game changer that will save lives and a tremendous change in the way we will manage this very, very complicated disease,” said Dr. Howard Riina, director of the Center for Stroke and Neurovascular Diseases at NYU Langone Health.
The guidelines were published Wednesday in the Association’s journal, Stroke, and released during the American Stroke Association’s International Stroke Conference 2018.
Michelle B., Encinitas, CA
Once in a great while our paths cross with an exceptional person and company. AIPRemodeling is one of them. Tyler Owen, the owner, is a professional in every sense. In addition to being a stellar contractor, he also has a deeply creative design ability. He is meticulous in both his and the work of his team. Tyler not only understands all the specific needs of someone in a wheelchair, but also understands the desire to create a beautiful home. He combines both seamlessly. From minute one, Tyler listened intently to what we wanted and then was able to add ideas that we never imagined. He respected our views and told us what would work. He carefully created designs, arranged many meetings to discuss and alter plans, was very transparent about every aspect of the job and worked patiently and endlessly with us from start to finish. Tyler does not cut corners, he produces a very high quality product. He offered his ideas and opinions as we went along. Also Tyler is a humble master craftsman himself and builds beautiful custom woodwork himself. Tyler is also meticulous and very fair in his bids and contracts. Whenever there was the inevitable addition/change that was not already in the budget, Tyler let us know immediately what the additional cost would be and executed a change order. No surprises or unknowns (the biggest blessing when working with a contractor). He is very generous in every way. Tyler has a team of employees who are very talented and competent in their craft, extremely kind and respectful at all times and always welcomed our presence and comments. Everything was neat and clean at the end of each day. Both my husband and I have only the most positive feelings about choosing and working with Tyler and his entire company. Everyday when we walked into the house, we appreciated the beautiful high quality work in our home. The entire process was a pleasure. Highly highly recommend.
Description of work:
Total wheelchair accessible renovation of our home including bathrooms, kitchen, revising the floor plan, walls down, widening hallways and doorways, creating accessible patios, windows and doors, drywall, painting, inside and out, basically turning our 30 yr. old home into a brand new house.
Jean K. – Oaks North, Rancho Bernardo
I highly recommend AGING IN PLACE who did a fantastic job of upgrading our bathroom, as well as other parts of the house. Fine owners who are long-time residents of the RB/Poway/Temecula areas…www.AIPRemodeling.com; C: 858-776-8700; P: 951-760-6728; F: 951-304-3709. Can’t praise them enough! J, Kunberger, Oaks North
Susan and Bob
We are so impressed! The day has run so smoothly. Your team has been professional, organized, careful, and jovial. Cleanup was immaculate!
We feel very fortunate to have AIP making this vision come true. Thank you.
Looking forward to tomorrow; one wonders how many people going through such a project say that.
Don’t Wait Until It’s too Late
Many times we have heard that people “aren’t ready” for our services yet. Or “I don’t need you yet”. We think you should WANT us BEFORE you NEED us. If you NEED our services it generally means that you have already experienced the traumatic injury and your mobility and accessibility to parts of your home have been hindered. So the time to install the grab bars and accessible bathing options is now.
The most common injury from a slip and fall in an elderly person is a broken hip. With a broken hip, according to one source, the average hospital stay is 7 days. While in the hospital you are at added risk for infection and pneumonia. Of course there is the pain. But we can’t really put a dollar amount or any other form of measurement on pain. We just all know we would like to avoid it at all costs. With a broken hip there will be the pain from the injury itself, the pain following the surgery and the pain experienced during the long months of exercise and rehab.
During recovery your mobility will also be limited. Little things we take for granted will have to be carefully monitored like sitting, bending, twisting or crossing your legs. You will even have to be careful with how you lie in bed and sleep. The list of restrictions does not end here.
So we say, do everything you can to avoid the fall in the first place. Having your grab bars installed now doesn’t mean you are getting older, it means you are getting smarter. It means you are ahead of the pack. While those around you are working through their recovery you can be enjoying your time and money on fun activities.
I don’t know about you, but I would much rather spend a few hundred dollars to have the grab bars installed, then spend the rest of the time and money on something I really love to do.
How To Make Your Home Safer
About half of all falls happen at home. To make your home safer:
- Remove things you can trip over (like papers, books, clothes, and shoes) from stairs and places where you walk.
- Remove unnecessary furniture or other items. We know this isn’t easy and can sometimes seem like an overwhelming task. If you need help there are great companies in the San Diego / Riverside area that will help you keep the items you want/need and to remove the items that you don’t. If you are helping an elderly parent/friend/relative sometimes this is the hardest thing to do. Allowing a 3rd party to assist you will remove the tension and let you get back to what you really need to be doing, taking care of a loved one.
- Remove small throw rugs or use double-sided tape to keep the rugs from slipping.
- Keep items you use often in cabinets you can reach easily without using a step stool.
- Have grab bars put in next to your toilet and in the tub or shower.
- Use non-slip mats in the bathtub and on shower floors.
- Reduce the step-over height to get into and out of your shower. There are easy and affordable options to have this done. Some that even preserve the bathing (as opposed to showering) function of your bathtub.
- Make your shower a low-threshold or no-threshold shower. Again, there are low cost, easy options for having this done. Most shower remodels can be completed within 2 – 3 days.
- Improve the lighting in your home. As you get older, you need brighter lights to see well.
- Hang light-weight curtains or shades to reduce glare.
- Have handrails and lights put in on all staircases.
- Wear shoes both inside and outside the house.
- Avoid going barefoot or wearing slippers.
- Have threshold ramps installed so you don’t catch your foot on the sliding door trim.
Next time we will talk about the “right time” to have the grab bars and other safety items installed.
Four Things You Can Do To Prevent Falls
As some of you may have already read, the concept behind Aging-In-Place Remodeling began forming about 17 years ago after Tyler was injured during a rock climbing accident. His back was broken and he was told that he would never walk again. As a 22 year old college student this news was devastating. However, since Tyler was a very healthy athlete in great condition, he was able to prove the doctor wrong and did indeed make a full recovery. This did not happen overnight though. It took many months of rehab and hard work. During those months he lived in a home that presented many obstacles. It is experiencing these obstacles first hand that give Tyler and Aging-In-Place Remodeling a distinct advantage in this field. We understand what people are going through and truly want to help them avoid the difficulties that Tyler faced.
While Tyler was injured during a rock climbing accident, many serious injuries occur within or near the home. A simple slip and fall can turn into a broken hip, a long hospital stay, and an even longer and more painful recovery. There are some simple ways to help prevent the slip and fall.
According to the CDC:
Many falls can be prevented. By making some changes, you can lower your chances of falling.
Four things YOU can do to prevent falls:
1. Begin a regular exercise program
Exercise is one of the most important ways to lower your chances of falling. It makes you stronger and helps you feel better. Exercises that improve balance and coordination (like Tai Chi) are the most helpful. Lack of exercise leads to weakness and increases your chances of falling. Ask your doctor or health care provider about the best type of exercise program for you.
2. Have your health care provider review your medicines
Have your doctor or pharmacist review all the medicines you take, even over-the-counter medicines. As you get older, the way medicines work in your body can change. Some medicines, or combinations of medicines, can make you sleepy or dizzy and can cause you to fall.
3. Have your vision checked
Have your eyes checked by an eye doctor at least once a year. You may be wearing the wrong glasses or have a condition like glaucoma or cataracts that limits your vision. Poor vision can increase your chances of falling.
4. Make your home safer
Our next Blog will talk about making your home safer. So make sure you check back soon.